Colon cancer is the second leading cause of cancer death in both men and women.
As a possible alternative to colonoscopy, a new home test is coming out.
To talk about them is Dr. Cynthia Rudert, a board-certified gastroenterologist in Atlanta, Georgia. She’s been involved in colon cancer screening and treating celiac disease for over 25 years. She’s also a Medical Advisor for the Celiac Disease Foundation, the Gluten Intolerance Group of North America, and Medical Director of the Atlanta Gluten Intolerance Group (GIG), and the Gluten Free Certification Organization (GFCO).
Dr. Mache Seibel: Colon cancer is a bad disease when it gets advanced; but there is the possibility of finding it early and potentially preventing it. Could you share a little information about that?
Dr. Cynthia Rudert: You’re exactly right, Dr. Seibel. It is the second leading cause of cancer death in both men and women, and it is highly preventable when it’s caught early. It’s also the most preventable cancer, but a lot of people eligible for colon cancer screening are not getting screened.
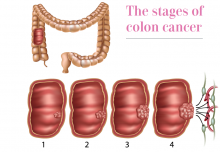
Dr. Seibel: Can you explain why it’s preventable because I think people don’t realize that there are steps to developing colon cancer and they can be diagnosed before colon cancer starts.
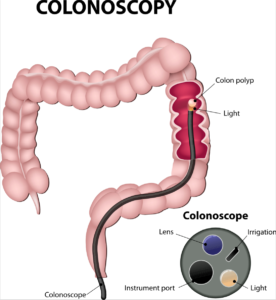
Dr. Rudert: Yes, of course. Colon cancer is preventable because it starts typically as a polyp, and polyps are benign, very tiny and they are visible when you look inside the colon with the colonoscope, which is a long flexible tube with a camera on the end, and that allows you to look at the polyps and to remove them. It takes about 10 to 15 years for a polyp to grow big enough to become a malignancy; so you have a long lag time in order to find these lesions.
Dr. Seibel: So, these little fleshy benign growths on the inside of the colon progress in size over 10 or 15 years, and eventually, they change from benign to borderline malignant to malignant tumors that actually can be found when they’re still benign and snipped out.
Dr. Rudert: Correct. And you want to get them when they’re small and easy to remove, because when they are larger and become cancerous, that’s when your life expectancy and the 5-year survival goes from over 90% to lower than 12%. You have a long time to make a huge difference.
Dr. Seibel: Basically, you go from a 9 out of 10 chance of being cured with early diagnosis, to 1 out of 10 chance to being cured late; so that’s a huge difference from likely to cure it, to more not likely to cure it.
Dr. Rudert: That’s exactly correct, and here’s why the majority of people wait a long time to do a colonoscopy: worry, concern about complications, sedation. People are human and don’t want to go in for something when they’re feeling great, and that’s exactly the time you should be screened.
Dr. Seibel: People are embarrassed. My patients say, “I don’t want to think about having a tube poked up my butt.” And they don’t want to think about all those medicines to clean them out; it’s messy, it’s uncomfortable, and it’s got a high yuck factor.
Dr. Rudert: It does. And I do a lot of second and third opinion consults, and it’s amazing the number of people who refuse to be screened. It’s estimated that there’s 23 million Americans that are eligible for colonoscopy that are not getting one. That’s 1 out of every 3 eligible people refusing to have a colonoscopy.
Dr. Seibel: Who should be screened for colon cancer?
Dr. Rudert: Screening is recommended by the American Cancer Society and the Gastroenterology Organization to start on individuals without symptoms at the age of 50; earlier than that if you have a family history, and for African-Americans, 45 years of age. That’s when you should get your first screening.
Dr. Seibel: This is men and women?
Dr. Rudert: Men and women, correct.
Dr. Seibel: So, if you’re 50 and no family history, you’re just a person that happens to be alive at age 50, male or female, you should be getting screened for colon cancer. If you have someone in your family with colon cancer, you should be getting screened at age 40. And, if you’re African-American because of an increased risk, age 45 would be the time to have a colonoscopy.
Dr. Rudert: Absolutely.
Dr. Seibel: We realize that because of embarrassment or for a variety of personal or other reasons, not everyone’s going to do a colonoscopy. You mentioned 23 million eligible people in the United States don’t get a colonoscopy. Is there a screening that people can do, if for whatever reason they choose not to get a colonoscopy?
Dr. Rudert: There is stool DNA testing. A study on DNA testing was published in the New England Journal of Medicine in 2014 by a group out of Mayo Clinic led by David Ahlquist. They partnered with Exact Sciences to develop the test.
Dr. Seibel: Stool DNA testing means that they test the stool for cancer genes, right?
 Dr. Rudert: Exactly. Those little polyps that you call in your colonoscopy song “bumps in the road” of your colon shed microscopic cells into the stool. Those microscopic cells coming from polyps or from cancers are abnormal; and so, you can collect the stool and actually look for the abnormal DNA in the stool and can predict those individuals with very high likelihood who will have a malignancy and also who will have a pre-malignant polyp.
Dr. Rudert: Exactly. Those little polyps that you call in your colonoscopy song “bumps in the road” of your colon shed microscopic cells into the stool. Those microscopic cells coming from polyps or from cancers are abnormal; and so, you can collect the stool and actually look for the abnormal DNA in the stool and can predict those individuals with very high likelihood who will have a malignancy and also who will have a pre-malignant polyp.
Dr. Seibel: So, basically, you’re mining the stool, the poop, for nuggets of DNA.
Dr. Rudert: Exactly.
Dr. Seibel: The test is not the same as looking at a polyp directly and saying “Wow! I see something.” How successful is the DNA testing?
Dr. Rudert: It will pick up 92% of all colon cancers. The FDA approved it in 2015, and when it was FDA- approved, Medicare approved it.
The test is called Cologuard, and it is a prescription stool test that must be ordered by a physician. It’s for folks with average risk that would be considering not having screening colonoscopy. Any physician can order it, and it’s actually sent via UPS to your home, and you collect the stool specimen at home and call UPS to come and get it and your doctor will have the results within about two weeks.
Dr. Seibel: It’s called Cologuard and it is 92% accurate. That’s not 100% compared to the direct inspection but still it’s very high and it gives people an option to discuss with their doctors if they don’t want to do have a screening colonoscopy.
Dr. Rudert: It also combines a stool blood test, so it has both tests together.
Dr. Seibel: So, it’s looking for blood in the stool as an indirect sign of cancer and DNA from shed cancer cells as a more direct sign of cancer. Of course you can have blood in your stool for instance because you have a fissure or a crack in the tissues around your rectum or from a hemorrhoid or from ulcerative colitis or many other kinds of diseases. Blood is just a warning sign; it’s not a guarantee of cancer.
Dr. Rudert: Exactly. It’s a warning sign when you have blood, that’s why just the regular stool testing for blood is not very sensitive.
Dr. Seibel: So, when you go in every year and you get your annual exam, your doctor may put a finger into the bottom side and get a little bit of stool and check it for blood, but those tests are much less accurate.
Dr. Rudert: Much less accurate because as you say it could be positive from a hemorrhoid or a fissure, or a variety of other reasons, and I think that’s why a lot of people are scared when they have a positive blood test; they think cancer. But it’s less likely to be cancer than some other problem she could potentially have.
Dr. Seibel: Are there other tests or anything else that you feel that people would benefit from knowing?
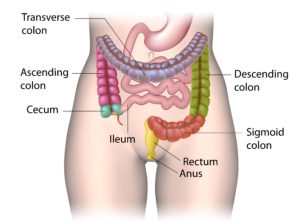
Dr. Rudert: There’s no other “at home test” on the market or even soon to be on the market, and this “at home test” is available everywhere from the Mayo Clinic to your local physician’s office. There is other testing, such as a flexible sigmoid exam. It isn’t very accurate because it can only see the very bottom part of the colon; it doesn’t look at the whole thing.
Dr. Seibel: The colon or large intestine is about 6 feet long. The small intestine, which comes before it, is about 20 feet long or more. And how much of the large intestine does the flexible sigmoid exam see?
Dr. Rudert: About a foot or so, and then you would be falsely reassured if that was normal, but you’re only looking at a small percentage of the entire colon.
Dr. Seibel: Well, I want to thank you very much for, let’s say, shedding light on this subject.