
Sadness is a normal emotion; but clinical depression is a disease that requires treatment. Do you know the difference? Here’s how to correlate depression and menopause.
When 52-year-old Ms. S made an appointment with me, a psychiatrist, things weren’t going well for her. Even seeing her grand-children wasn’t bringing a smile to her face. She “felt ‘blah’ all spring,” her usually favorite time of the year. She’s had trouble sleeping and didn’t have her usual energy so she didn’t plant the flowers or tend to the garden that brings her great pride. She can’t concentrate on her romance novels, and just feels her life is meaningless; asking “What’s the point?”. She stopped calling her daughter, stopped attending her book club and resigned as head of the town gardening group. Her husband says, “She’s moving as slow as molasses these days.” She told me that in the past she felt really sad both after the birth of her first daughter and when she moved to a new town away from her family of origin. She’s never taken medication for mood before. She last menstruated about nine months ago and has hot flashes nearly every day.
 Perhaps you can tell from her story that Ms. S sounds like she is in perimenopause and has clinical depression, or what psychiatrists call a major depressive episode. There are three different “kinds” of depression that are all very different. According to the North American Menopause Society:
Perhaps you can tell from her story that Ms. S sounds like she is in perimenopause and has clinical depression, or what psychiatrists call a major depressive episode. There are three different “kinds” of depression that are all very different. According to the North American Menopause Society:
A depressed mood is a normal, brief period of feeling blue or sad that is commonly experienced and rarely requires treatment. The medical term is dysphoria.
Depression as a symptom — sometimes called an adjustment reaction, and can be caused by a many types of medical or psychological problems, or to intense reactions to life events (such as divorce, losing a job, death of a loved one). It is usually short term and most often does not require treatment, although it can progress to clinical depression.
Clinical depression — is a pervasive mood that causes serious disruptions to a person’s ability to function. This is a disorder believed to result from a chemical imbalance in the brain. A clinical (major) depression requires treatment. According to the National Institutes of Mental Health, brain-imaging technologies, such as magnetic resonance imaging (MRI), reveal that the brains of people suffering from depression look different than those of people without depression. The parts of the brain responsible for regulating mood, thinking, sleep, appetite and behavior don’t appear to be functioning normally. In addition, important neurotransmitters – chemicals that brain cells use to communicate – appear to be out of balance.
We define a depressive episode when a person has five or more of the following nine symptoms present most days for at least two weeks. At least one of the symptoms must be either depressed mood or loss of interest or pleasure.
- Feelings of depressed mood
- Inability to experience pleasure in most activities*
- Significant unintentional weight loss or weight gain or decrease or increase in appetite
- Not being able to fall asleep or stay asleep or sleeping too much*
- Being fidgety and restless or moving very slowly*
- Fatigue or loss of energy*
- Feelings of worthlessness or excessive or inappropriate guilt*
- Difficulty thinking or concentrating on things, finishing tasks, or making decisions*
- Thoughts of death, that you would be better off dead, or making plans to end your life
The brains of people suffering from depression look different than those of people without depression
Ms. S has the six symptoms of depression starred above for over two weeks that have negatively affected her functioning. Those findings mean she meets the medical criteria for the diagnosis of a major depressive episode.
I told her that women have depression up to twice as often as men. Women undergoing the menopausal transition or perimenopause – when menstrual cycles becomes irregular – are at an even greater risk of depression, even if they have never had depression in the past. Ms. S likely had some sadness adjusting to difficult situations (new town, becoming a mother) but not a clinical depression in her past.
While it is normal to have brief periods of feeling a bit down or blue, especially when life is stressful or involves change, clinical depression is severe and constant. It is not unusual for a woman to experience sadness in reaction to the loss of a loved one, job loss, or other significant loss. But sadness or grief does not affect self-confidence nor desire to live the way clinical depression does. Depressive symptoms can also be caused by medical conditions, such as thyroid disorder, or excessive alcohol and substance use.
Clinical depression is different from sadness or grief. Clinical depression includes an all-encompassing mood of feeling depressed, sad, hopeless, or discouraged. Some people may experience ongoing lack of pleasure and interest in the activities that used to be enjoyed. In clinical depression, depressive symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning. Some women also notice an increase in physical symptoms such as headaches, stomach aches or increased pain.
Treatment for Clinical Depression
If you feel you may be suffering from depression, first make an appointment to see your doctor. He/she will do a thorough history and physical exam to be sure that these feelings are not being caused by a medical condition. Other mental health disorders can present in similar ways, such as anxiety disorders, so it is important to see your physician so that you can be properly diagnosed.
Once a diagnosis of depression is made, your physician can discuss treatment options with you and determine which one(s) may be best from suited for you.
 Options for treatment include:
Options for treatment include:
- Antidepressant medications
- Psychotherapy
- Aerobic exercise
- Complementary therapies
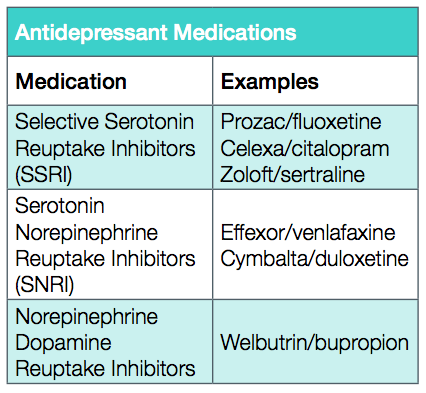
Antidepressant medications and psychotherapy have the best evidence for effectively treating clinical depression. Healthy behaviors such as exercise, healthy diet and some supplements (example vitamin B6, omega three fatty acids/fish oil, St. John’s wort, SAMe) may be of benefit in reducing sadness. There are many anti-depressant medications to choose from and in general they have very few side effects. Most antidepressants take 4-6 weeks to have a full effect. Also, Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) both reduce hot flashes!
The increased risk of depression in perimenopause begins to decrease in the postmenopausal period
Ms. S and I discussed the above options for her care. She was initially reluctant to take medication for her mood.
I explained to her that SSRI medication also reduces hot flashes and she decided to start an SSRI both for her mood and for her hot flashes. She also wanted to begin therapy with the intent of learning ways of thinking and behaving to improve her mood.
There is no “one size fits all” treatment plan, so it is best to work closely with your physician to find what works best for you. This may include trying more than one antidepressant medications or finding a combination of treatment options. For most women, with treatment they will gradually feel better. And the increased risk of depression in the perimenopausal period begins to decrease in the postmenopausal period.
_______________________________________
Wendy Marsh MD MSc and Shaula Woz MD,
Department of Psychiatry, University of Massachusetts Medical School
References
1. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013. Web. [access date: 1 June 2013]. dsm.psychiatryonline.org.
2. Clayton AH, Ninan PT. Depression or Menopause? Presentation and Management of Major Depressive Disorder in Perimenopausal and Postmenopausal Women. Prim Care Companion J Clin Psychiatry. 2010; 12(1): PCC.08r00747.
3. Women and Depression: Discovering Hope. National Institute of Mental Health, 2009. Web. [access date: 1 June 2013].
http://www.nimh.nih.gov/health/publications/women-and-depression-discovering-hope/index.shtml






